Rep. John Murtha (D-PA) died yesterday, a week after routine gall bladder surgery (cholecystectomy). He was a powerful congressman with his finger on the button of Pentagon appropriations.
And with his high-profile death comes an opportunity to explore some medical malpractice issues.
So let’s do this in Q & A form:
What is the first reaction as to why this happened?
First up is the most common reason for malpractice litigation with gall bladder surgery: That the common bile duct was mistakenly cut. I don’t know what happened here, of course, since I don’t have the medical records or the autopsy results, but you can bet that is one of the first places people will look.
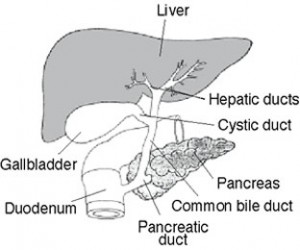 As basic background, the liver produces bile that helps us digest. It is transmitted to the intestines via ducts. The gallbladder stores bile. A schematic is seen here at left.
As basic background, the liver produces bile that helps us digest. It is transmitted to the intestines via ducts. The gallbladder stores bile. A schematic is seen here at left.
Was this due to infection, instead of a common bile duct injury?
Some are claiming that the death occurred because the intestine was mistakenly cut during surgery, and that this caused an infection. Someone investigating the case would then naturally ask the following questions:
Was the cut intestine noticed during surgery, and if not, why not? Cutting something that you’re not supposed to cut is one thing. But failing to notice that it was cut is a whole different thing. This is often the dividing line between when a malpractice case is successful or not. Bad results by themselves don’t mean malpractice. Failing to recognize mistakes, however, is a different concept entirely.
If noticed during surgery, what was the response? This surgery was done via a laparoscope, in which the scope is passed through a small incision, with surgery done with a camera-assist. Depending on when and where the bad surgical cut happened, and whether it was noticed at the time, the logical questions are who, if anyone, was called in to assist in the repair and how was it done?
When were the first signs and symptoms of infection noticed and reported and what was done about it? If the cut was noticed during surgery, then in addition to any potential antibiotics that may have been given, would have been very strict discharge instructions to the patient on the signs and symptoms of infection and the critical nature of prompt action.
If this is a known risk of the procedure, why blame the doctor?
This one is a classic, and defendants love it in the courtroom. But it is the wrong question to ask. The issue is not whether something was a known complication or risk, but whether it was avoidable with good care.
Think of it this way: Is a car accident a risk of driving? Does the fact that accidents are a risk of driving mean that the guy who ran the stop sign is not responsible?
Was Murtha just one of up to 98,000 estimated deaths from malpractice in the US each year (Study: To Err is Human)? Time will tell on that one. And we will see to what extent if death has an effect on the health care debate in Congress and the desire by some to grant certain immunities to the medical industry for malpractice.
On a last note, not only was Murtha deeply involved in political-military issues, but the surgery took place at the National Naval Hospital in Bethesda, MD. This adds another potential political element to any investigation or legal action in the event that family moves in that direction.
Eric:
Did you ever learn the scientific method?
Your "reference" was medicalnews today. The link to the complete study at healthgrades did not work. Most importantly, I went to pubmed. This "study" has never been published in a peer-reviewed journal.
Other healthgrade press releases (I can use google too eric):
"The report further suggested that those patients who experience an error in treatment or care at a hospital have a one in four chance of dying from the mistake. In total, HealthGrades said, 247,662 patients studied between 2003 and 2005 died from potentially preventable problems."
It seems that healthgrades is increasing their numbers by 25% every couple of years eric. Is that true? I don't know, you don't know, nobody really knows as nothing has actually been published in a peer-reviewed journal.
One of the two references I listed was a peer-reviewed article. The other was an editorial by one of the primary articles in which "to err is human" extrapolates it's data from, bringing up flaws in his own study. The point eric is the confusion at multiple levels on defining this subject. Sadly, you are not interested in discussing the subject, you are interested in ATLA talking points for your own bottom line.
PS: Another thing
"One big problem in doing any study, of course, is that only the doctor's point of view is used since the patient is dead."
The doctor involved in the death is not interpreting the data in the study (including to err is human). I don't even know what point you are even trying to make here except to pull on heart-strings. Will you start channeling dead babies for an encore?
I am a general surgeon and I routinely perform this type of gallbladder surgery. While it is possible to injure adjacent structures during surgery, it is not as likely with routine surgery as it is during an emergent gallbladder procedure where the gallbladder and adjacent structures are inflamed. It is possible that he had chronic adhesions on his gallbladder and maybe his colon was adherent to the gallbladder and when the surgeon peeled the colon away from the gallbladder a small rent was made in the colon. Only speculation since I have not heard how this colon injury occurred. Presumably, the patient would have been in a lot of pain postoperatively, so not sure what was the delay in getting him treated sooner.
It seems that healthgrades is increasing their numbers by 25% every couple of years eric. Is that true? I don't know, you don't know, nobody really knows as nothing has actually been published in a peer-reviewed journal.
I mentioned the report in a comment simply to indicate that there are others trying to study the same issue, and the numbers could vary widely due to the difficulty studying it. Since the patient is dead, researchers are forced to rely on the doctor's version of events in the medical records.
The doctor involved in the death is not interpreting the data in the study (including to err is human). I don't even know what point you are even trying to make here except to pull on heart-strings. Will you start channeling dead babies for an encore?
Nobody said the doctor was interpreting data. The doctors create data (the medical chart). Plenty of medical charts are written from a CYA perspective. But the patient's point of view sometimes differs, and that would not be reflected.
And that is a problem that is difficult to research and leads to estimates by researchers that are easy to criticize.
But that doesn't mean the studies shouldn't be done and that doesn't mean that the estimates are off.
It is possible that he had chronic adhesions on his gallbladder and maybe his colon was adherent to the gallbladder and when the surgeon peeled the colon away from the gallbladder a small rent was made in the colon. Only speculation since I have not heard how this colon injury occurred.
There is no question that we are left with speculation in the wake of his death, since we don't have the chart and certainly don't have Murtha's input.
I've worded the entire posting as a series of questions since, I think, it would be unfair to do otherwise at this point.
As a retired Marine, treated in a military medical facility, wouldn't his estate be prohibited from suing under Feres?
I've never litigated a Feres doctine case, though I thought it dealt with active duty service members being barred from suing, and Murtha was retired.
Certainly I would welcome more commentary on that subject if you have support for preclusion of suit.
deleted
re:" mentioned the report in a comment simply to indicate that there are others trying to study the same issue, and the numbers could vary widely due to the difficulty studying it. Since the patient is dead, researchers are forced to rely on the doctor's version of events in the medical records."
Eric do you understand the difference between a private company (healthgrades) "publishing" it's data on it's website versus a critically evaluated research study published in a peer-reviewed journal including methods and material, results, statistical analysis for all to read? Do you even understand the scientfic method eric?
"Nobody said the doctor was interpreting data. The doctors create data (the medical chart). Plenty of medical charts are written from a CYA perspective."
Though I agree doctors can "flavor" their bias in the chart, The fact is laboratory results don't "lie", Microbiology tests don't "lie", pathology results don't "lie". The results are what they are (unless you are accusing somebody of doctoring the results counsler). The whole purpose of these studies whether it be to err is human or the other one which I linked (and which you obviously still have not read) is to attempt to take bias out of the equation. However, these are all retrospective studies which by definition will have issues that prospective studies do not.
re:
"But the patient's point of view sometimes differs, and that would not be reflected"
Again what is your point here eric? These are supposed to be independant studies that are rigourously evaluated without doctor or patient bias. What the patient (or family) "thinks" is not the issue. The question is whtether medical error contributed to a patient's death. This is science eric not law. Scientist's take a dim view of legal antics such as parading an injured (whether or not it was malpractice) patients in front of jurors to pull on heart strings. We don't channel dead babies in science eric. Sadly from what I can tell, you have very little understanding of the scientific method.
goodbye.
What the patient (or family) "thinks" is not the issue.
Nor did anyone say it is. Since you've missed the point, I'll try again by putting this into a real-life situation:
28 yo woman goes to OBGYN and complains of a hard breast lump.
MDs says don't worry about it. No biopsy.
A year later the cancer is found. MD claims that prior exam showed fibrocystic breasts. Pt says hard nodule was shown to MD.
This type of scenario plays itself out in a hundred different ways in a doctor's office or hospital.
This is not a question of what the patient "thinks" but of what the patient complained of. That would be data, but only if the data was properly recorded.
And there is no study in the world that could resolve the conflict by looking at the medical records. Even with full blown trials with live witnesses it can be tough.
So studies of the issue have built-in problems, and lead by definition to estimates.
A scientific study is built on empirical data. That data is often missing, or the data is disputed (MD says one thing, pt says something else, but only MD chart is used).
And no matter how hard you try, writing in an obnoxious style won't cure that deficit in the data. We are left with estimates.
Criticizing is, therefore, easy. Building a better way to study the problem is not.