 Dear New York State Legislators:
Dear New York State Legislators:
Deeply hidden from public view inside a report from the New York State Department of Health is a proposal to place an artificial $250,000 cap on medical malpractice pain and suffering claims. That report was given to Gov. Andrew Cuomo last week. The proposal is tucked inside something called the Medicaid Redesign Team, and was authored by insurance companies and medical institutions. There were no patient representatives on the committee.
You should soundly reject this anti-consumer bill on both public policy and monetary grounds.
First, a quick review of our current system before we get to the policy stuff: New York already has caps on personal injury cases for those runaway verdicts you see in the papers from time to time. These are not artificial, one-size-fits-all caps, but caps that are specifically geared to the individual cases. New York has successfully been doing this for almost 200 years for verdicts that are unreasonable, since Chief Judge James Kent wrote the following in Coleman v. Southwick in 1812:
“It is not enough to say, that in the opinion of the court, the damages are too high and that we would have given much less. It is the judgment of the jury, and not the judgment of the court, which is to assess the damages in actions for personal torts and injuries….The damages, therefore, must be so excessive as to strike mankind, at first blush, as being beyond all measure, unreasonable and outrageous, and such as manifestly show the jury to have been actuated by passion, partiality, prejudice, or corruption. In short, the damages must be flagrantly outrageous and extravagant, or the court cannot undertake to draw the line; for they have no standard by which to ascertain the excess.”
The standard is no longer “flagrantly outrageous and extravagant.” Now it reads, “deviates materially from what would be reasonable compensation” that is codified in section 5501(c) our Civil Practice Law and Rules:
In reviewing a money judgment in an action in which an itemized verdict is required by rule forty-one hundred eleven of this chapter in which it is contended that the award is excessive or inadequate and that a new trial should have been granted unless a stipulation is entered to a different award, the appellate division shall determine that an award is excessive or inadequate if it deviates materially from what would be reasonable compensation.
So a complainant not only needs to win the case before the jury, but that verdict then gets reviewed by the trial judge and then can be reviewed again by an appellate court. In other words, the system we currently use has a both a belt and suspenders to keep it from falling down.
What is the advantage of changing a system that isn’t broken? Well, by limiting the right to a trial by jury, it gives a healthy dose of immunities and protections to those that committed the wrongful acts. Is that an advantage? It is if you are the one trying to evade responsibility for your conduct.
If the artificial cap is in place, the injuries won’t be diminished. The only thing that will change is that the economic burden of those injuries will be borne by the victim instead of the party that caused them. Is it sound public policy to victimize the injured person a second time? Is it good public policy to discard the concept of personal responsibility?
At the moment, only the most severe injuries are the subject of malpractice suits. This is true for two reasons. First, the suits are very expensive to bring. There is little point bringing an action whose reasonable value might be $50,000, if it will cost that much in experts, records and depositions to get to verdict. And second, New York currently has some of the lowest attorneys fees in the nation as a result of “reforms” you enacted in the mid-1980s. Those fees start at 30% of the first $250,000 and rapidly slide down to 10% of anything over $1.25M. In other words, complex and expensive malpractice cases have lower legal fees than the norm, causing a predictable drop in the number of attorneys willing to undertake the difficult cases.
The result of that “sliding scale” fee structure is that doctors and hospitals in New York already enjoy a significant amount of immunity from medical malpractice cases. It is simply not cost effective to bring many of the actions that present themselves to our doors, even if they appear to have merit. Most lawyers that practice in this area, myself included, will reject at least 95-98% of the inquiries to the office.
The insurance companies and medical profession now ask you to give them a second giant helping of immunity by eviscerating the pain and suffering damages. The ones that will be hurt, of course, are those who have been most seriously hurt. It will have no effect on frivolous cases, as they do not have a value over $250,000. They have a value of zero.
And it isn’t as if granting such immunities and protections will lower the incidence of malpractice, which already causes up to 98,000 deaths a year according to the Institute of Medicine. If the government wants to cut Medicaid costs, and cut lawsuits, the efforts must be devoted to safety, not killing patient rights. Telling people they can act with impunity doesn’t increase safety.
If the top pain and suffering award is only $250,000 — which sounds like a lot if you grew up in the Great Depression but means quite a bit less when a surgeon wants $5-10,000 to come in to court and testify for a morning — the effect will be courthouse doors being slammed shut in the faces of many people. Any case with even modest complexity will be rejected by attorneys, and the victim left to suffer without compensation.
And not only is this lousy public policy, but it also makes no economic sense. What happens to someone crippled by malpractice? Generally, they can’t work anymore or raise their children if they have them. They also may be uninsurable due to their pre-existing conditions. Who pays when the injured person is poor? That’s right, the public does in the form of tax dollars going to various welfare and Medicaid programs.
But if Big Hospital, Inc. commits malpractice and injures someone, why should the taxpayers be saddled with these burdens? Why shouldn’t the hospital be paying for the damage it caused? Ultimately, of course, someone will pay, and it sure makes more sense that the one that did the damage should pay the bill and not the victims or taxpayers.
Were you worried about the costs of malpractice to medical care? Don’t worry too much. For the costs are less than 1/2 of one percent.
In sum, this proposal crafted by insurance companies and medical institutions is not only anti-consumer, but will saddle taxpayers with burdens caused by others. It makes no sense on public policy grounds or economic grounds. There will, however, be a windfall profit for the insurance companies and those doctors that hurt the most people and make the biggest mistakes.
For more on the subject:
State Bar Blasts Proposal to Cap Medical Malpractice Awards (New York Law Journal)
The New York State Bar Association and its president yesterday blasted a recommendation by Governor Andrew M. Cuomo’s Medicaid reform task force to cap medical malpractice awards for non-economic losses at $250,000.
Such caps are “anathema with respect to equal protection/access to justice,” the state bar’s Committee on the Tort System said in a memo in opposition to the Medicaid Redesign Team’s recommendation. The memo was endorsed by the bar’s executive committee….
How New York Caps Personal Injury Damages
…So why put arbitrary caps in place if common sense ones already exist? Because the movement to do so has nothing to do with finding justice, but rather, is run by big business and its front groups such as the U.S. Chamber of Commerce to give negligent conduct various forms of immunities and protections when folks are injured. The idea is to remove the concept of personal responsibility for one’s actions…
Medical Malpractice Insurers Price-Gouged Doctors During This Decade
Americans for Insurance Reform (AIR) announced today the release of Stable Losses/Unstable Rates 2007, a new study that examines fresh insurance industry data to determine what caused the most recent medical malpractice insurance crisis for doctors. The study by AIR, a coalition of over 100 consumer and public interest groups representing more than 50 million people, finds that the insurance crisis that hit doctors between 2001 and 2004 was not caused by claims, payouts or legal system excesses as the insurance industry claimed….
Medical Malpractice Economics
Two weeks ago I wrote Medical Malpractice – A Primer, directed toward members of the medical community due to a recurring theme I saw on medical blogs: The idea that such suits are brought cavalierly….
I promised a follow-up on how cases are selected by a plaintiff’s attorney, but first want to deconstruct the time and money needed if the matter is taken. For only by understanding the time and money risks can one appreciate the importance of careful screening for potential litigation…
The Medical Malpractice “Crisis” Hoax — From Public Citizen
…Good doctors, however, don’t seem to be the problem. Since 1991, according to the report, 5.9 percent of U.S. doctors were responsible for 57.8 percent of the number of medical malpractice payments. That is an extraordinary statistic.
A few other points from the report, and things to think about when someone advocates closing the courthouse door to those injured by negligence:
- The number of malpractice payments declined 15.4 percent between 1991 and 2005.
- Adjusted for inflation, the average annual payment for verdicts declined 8 percent between 1991 and 2005.
- Payments for million-dollar verdicts were less than 3 percent of all payments in 2005.
- Over 64 percent of payments in 2005 involved death, or major or significant injuries.
First, do no harm
…Two recent studies make it clear those policies have not been widely adopted. Last November, both the New England Journal of Medicine (NEJM) and the inspector general for the Department of Health and Human Services published results of studies showing that the level of risk to patients in our nation’s hospitals is at crisis levels, with hundreds of people dying daily from medical errors…
Do Texas Med-Mal Damage Caps Work? (What Do You Mean By “Work”?)
…But what, exactly does it mean for a statute to “work” when it reduces the ability of the most badly injured individuals to recover for their loss?
- Does offering government protectionism for tortfeasors mean it works?
- Does stopping those who’ve been victimized from recovering from their loss mean it works?
- Does destroying the concept of personal responsibility for one’s actions mean it works?
If the objective is to offer windfalls to those whose negligence has injured others then one might say it works. But that doesn’t makes it good public policy…
Child’s Feet and One Hand Amputated After Emergency Room Delay (California Tort “Reform” In All Its Glory)
…For out in California, they enacted a one-size-fits-all tort “reform” with a cap of $250,000 on non-economic damages (pain and suffering). The state did this in 1975. And it hasn’t changed in the last 35 years. Adjusted for inflation, it would be about a million dollars today. But it has never been adjusted.
That’s right, a lifetime of missing three limbs, if she survives, and this child might receive compensation of $250,000 for her pain and suffering. Less, of course, the money spent to hire the experts, take the depositions, get all the records, and get the case to trial after a few years, and paying the lawyers to do it. Assuming that lawyers can be found to put forth the money and absorb the risk for a contingent fee….
Does the Tea Party Believe in Conservatism or Tort “Reform”? (8 Questions)
As the Tea Party movement gains more attention, some folks want to know exactly what they believe in. Today’s question: Do they believe in a smaller, less intrusive, government or will they follow the Republican Party down the path of Big Government Tort “Reform”?
Since the Tea Party is a nascent and disorganized collection, I’m tossing out eight questions for those conservatives in the movement to ponder as they decide which side of the tort “reform” debate they are on…
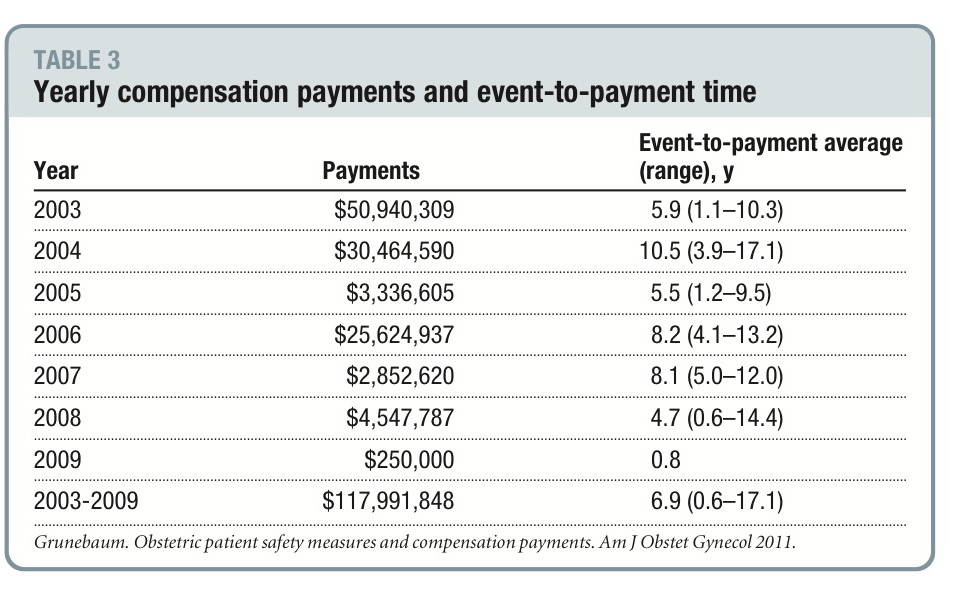 It is abundantly clear then, from a pure dollars and cents point of view, that the medical profession has a spectacular opportunity to save money by slashing its malpractice payments. But to do that, they have to improve patient safety. You can see the raw savings in the chart on the left.
It is abundantly clear then, from a pure dollars and cents point of view, that the medical profession has a spectacular opportunity to save money by slashing its malpractice payments. But to do that, they have to improve patient safety. You can see the raw savings in the chart on the left.

